Author
Reviewer
Share Article
Denosumab 101: Safety, Tolerability and Calcium Monitoring…..Oh My!
Safety, Tolerability and Calcium Monitoring…..Oh My!
| Author | Reviewer |
|
David Kendler, MD, FRCPC Professor of Medicine (Endocrinology) University of British Columbia Vancouver, BC |
Christine Palmay, MD, CCFP, FCFP Midtown Health and Wellness Clinic Toronto, ON |
Addressing patient safety concerns
It is of paramount importance that clinicians explain to patients the balance of risks and benefits of treating osteoporosis. Without this understanding, patients may see the risks of osteoporosis therapy as greater than the risks of not being treated with the goal of reducing fracture risk. Have patients consider that, although treatments for osteoporosis may have rare side effects, in patients at high risk of fracture, the “side effects” of not treating osteoporosis are fragility fractures. Such fractures deprive patients of quality of life, often resulting in dependency and institutionalization. In particular, with hip fractures there is a 23% one year mortality; patients after hip fracture very frequently do not return to their prior independent lifestyle. A loss of independence is not only life changing for both the patient and their families, but truly resonates with patients when they understand the severe consequences of a fracture.
Simply put, an osteoporotic fracture is more than a broken bone and affects all parameters of a patient’s life as well as their caregivers.
Watch this video summary with blog author Dr. David Kendler
What about atypical fractures?
The American Society for Bone and Mineral Research has issued guidance regarding the diagnosis of AFF and its management. It is important to recognize that not all subtrochanteric fractures are AFF,  and even with all characteristics present, approximately 30% of AFF patients have not been exposed to osteoporosis therapies. In addition to their subtrochanteric location and occurrence with minimal trauma, other features include propagation from a lateral cortical stress fracture, transverse orientation, lack of comminution, 50% bilateral involvement, and frequent prodromal thigh pain. Such fractures are indeed rare but accumulate in patients on longer-term bisphosphonate. The frequency of AFF decreases dramatically if long-term bisphosphonate users interrupt therapy for just one year, supportive of the benefit in selected patients of bisphosphonate “drug holiday”. Drug holiday should not be considered in patients on denosumab, since reversal of antiresorptive activity can be much more rapid.
and even with all characteristics present, approximately 30% of AFF patients have not been exposed to osteoporosis therapies. In addition to their subtrochanteric location and occurrence with minimal trauma, other features include propagation from a lateral cortical stress fracture, transverse orientation, lack of comminution, 50% bilateral involvement, and frequent prodromal thigh pain. Such fractures are indeed rare but accumulate in patients on longer-term bisphosphonate. The frequency of AFF decreases dramatically if long-term bisphosphonate users interrupt therapy for just one year, supportive of the benefit in selected patients of bisphosphonate “drug holiday”. Drug holiday should not be considered in patients on denosumab, since reversal of antiresorptive activity can be much more rapid.
![]() What are the implications of osteoporosis and fractures?
What are the implications of osteoporosis and fractures?
Doc, do my bones become brittle with long-term treatment?
The denosumab registration clinical trial continued patients from the original three year placebo-controlled trial on open label denosumab for a total of 10 years (FREEDOM extension). In patients on denosumab for 7 to 10 years, vertebral and nonvertebral fractures remained low despite aging of the patient population. Indeed, compared to the first three years of denosumab therapy, there was a further 25% reduction in nonvertebral fractures as patients continued denosumab treatment from the third to the 10th year. This was in association with the progressive increases in both spine and hip bone mineral density with longer-term denosumab therapy. There is no known limit to the length of time patients can remain on denosumab therapy. In summary, set expectations that osteoporosis is a chronic disease as such, often merits long-term treatment and regular ongoing assessment.
Ok, doc, but what is osteonecrosis of the jaw (ONJ) and how frequently does it occur?
 In osteoporosis clinical trials, ONJ is defined as a delay in dental healing of greater than eight weeks after conservative therapy has been implemented, usually after an invasive oral procedure. Such lesions usually heal after longer conservative management. The frequency of ONJ has been estimated at one in 50,000 individuals; the frequency may also increase with long-term antiresorptive therapy. Patients (and dentists) often have a perception that ONJ has much greater clinical consequences. Having discussions regarding the relative ratio of benefit to risk is essential and this may require communication with the treating dentist.
In osteoporosis clinical trials, ONJ is defined as a delay in dental healing of greater than eight weeks after conservative therapy has been implemented, usually after an invasive oral procedure. Such lesions usually heal after longer conservative management. The frequency of ONJ has been estimated at one in 50,000 individuals; the frequency may also increase with long-term antiresorptive therapy. Patients (and dentists) often have a perception that ONJ has much greater clinical consequences. Having discussions regarding the relative ratio of benefit to risk is essential and this may require communication with the treating dentist.
![]() How do we identify patients at high and very high risk of fracture?
How do we identify patients at high and very high risk of fracture?
What about HYPOcalcemia? Do I need to worry?
Potent antiresorptive therapy with denosumab or bisphosphonate may impair an individual’s ability to mobilize calcium from bone, especially in circumstances of enteral calcium or vitamin D deficiency. Osteoporosis clinical trials have not demonstrated increased risk of hypocalcemia in patients on antiresorptive therapy, perhaps because renal insufficiency patients are excluded, those patients with pre-existing hypocalcemia are managed prior to denosumab administration, and because all patients are given supplemental calcium and vitamin D. In clinical practice, hypocalcemia may occur in patients commencing denosumab or bisphosphonate therapy. With denosumab, clinical hypocalcemia may arise between five and 14 days after denosumab dosing. Since the timing is unpredictable, post dose calcium testing is problematic. For most patients, it is sufficient to inform them that they require medical attention if they experience perioral paraesthesia and muscle cramps, both of which can occur with hypocalcemia. Particular caution is advised for patients with malabsorption or chronic kidney disease and impaired conversion of 25 hydroxy vitamin D to its active metabolite 1, 25 hydroxy vitamin D. Such patients may benefit from calcium chemistries approximately seven days after their initial dose of denosumab.
Are infections a concern while on treatment?
Denosumab is a RANK ligand monoclonal antibody with its primary antiresorptive bone effects being the reduction of the formation, functioning, and survival of osteoclasts. Because RANK receptors also exist in immune tissue such as lymph nodes, infective complications in patients on denosumab clinical trials have been carefully monitored. The only infective complication seen in excess in 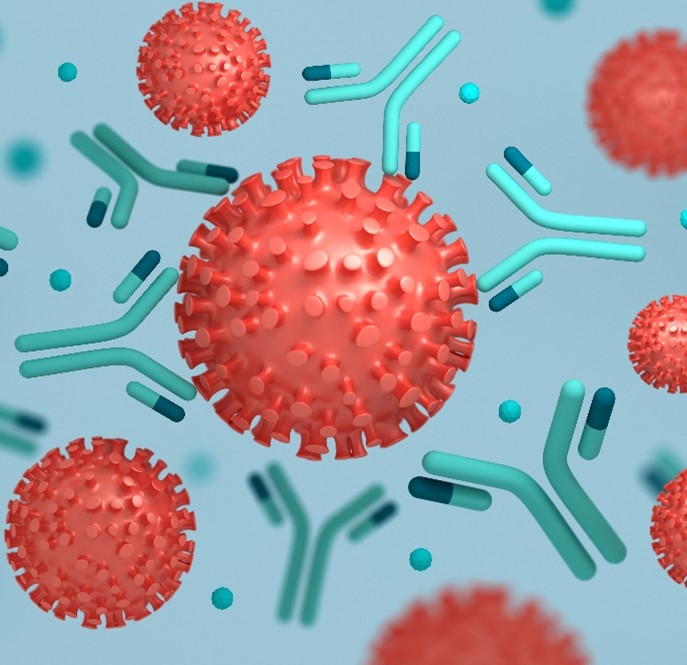 patients on denosumab compared to placebo is lower extremity cellulitis occurring in 12 denosumab patients and only one placebo patient in the first three years of study. Other infections are balanced between denosumab and placebo patients. As well, in the extension study up to 10 years, there was no increase in infections with longer-term therapy; hematologic parameters remained unchanged.
patients on denosumab compared to placebo is lower extremity cellulitis occurring in 12 denosumab patients and only one placebo patient in the first three years of study. Other infections are balanced between denosumab and placebo patients. As well, in the extension study up to 10 years, there was no increase in infections with longer-term therapy; hematologic parameters remained unchanged.
![]() How common is ONJ in Osteoporosis patients and how do I manage the risk?
How common is ONJ in Osteoporosis patients and how do I manage the risk?
Is it true that once denosumab therapy has been started, it can never be stopped?
As with other therapies for chronic disease (such as hypertension, diabetes, hypercholesterolemia), discontinuing treatment leads to a reversal of beneficial effects and return of patient risk for outcomes. With denosumab, inhibition of bone resorption begins to reverse around eight months after the last denosumab injection leading to increases in bone turnover, decline in bone density back to baseline, and rarely multiple vertebral fractures. For this reason, if denosumab needs to be discontinued, a bisphosphonate or other antiresorptive therapy should be introduced, subsequent to which a bisphosphonate drug interruption (drug holiday) may be feasible.
We have so much to deal with, why is this really important for my patients?
We must remind ourselves that osteoporosis is as significant as other chronic diseases, such as stroke or heart disease, but tragically is underdiagnosed and undertreated. Favourable patient outcomes require informed decision-making by both patients and their care providers. Without a good understanding of risks and benefits, osteoporosis patients may discontinue therapy or a failure to implement prescribed medications. For this reason, taking the time to explain risks and benefits of treatment will lead to better adherence to therapy in patients at high risk of fragility fracture and result in better healthcare outcomes. Remind patients it is not “just a fracture.” The fracture itself is a symptom of underlying disease and a possible herald for dramatic decline in quality of life.
Continuing learning with CCRN webcasts and podcasts:
![]() How can I apply a systematic approach to managing OAB? - *ACCREDITED WEBCAST*
How can I apply a systematic approach to managing OAB? - *ACCREDITED WEBCAST*
The development of this blog was overseen by the Canadian Collaborative Research Network and was supported through an educational grant from AMGEN.
References
Kendler DL, Cosman, F, Stad, RK. Denosumab in the treatment of osteoporosis: 10 years later: a narrative review. Adv Ther (2022) 39:58–74
Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–65.
Bone HG, Wagman RB, Brandi ML, et al. 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol. 2017;5:513–23.
Cummings SR, Ferrari S, Eastell R, et al. Vertebral fractures after discontinuation of denosumab: a post hoc analysis of the randomized placebo-controlled FREEDOM trial and its extension. J Bone Miner Res. 2018;33:190–8.
Lamy O, Gonzalez-Rodriguez E, Stoll D, Hans D, Aubry-Rozier B. Severe rebound-associated vertebral fractures after denosumab discontinuation: 9 clinical cases report. J Clin Endocrinol Metab. 2017;102: 354–8.
Kendler D, Chines A, Clark P, et al. Bone mineral density after transitioning from denosumab to alendronate. J Clin Endocrinol Metab. 2020;105: e255–64.
Watts NB, Grbic JT, Binkley N, et al. Invasive oral procedures and events in postmenopausal women with osteoporosis treated with denosumab for up to 10 years. J Clin Endocrinol Metab. 2019;104: 2443–52
Khan AA, Morrison A, Kendler DL, et al. Case-based review of osteonecrosis of the jaw (ONJ) and application of the international recommendations for management from the International Task Force on ONJ. J Clin Densitom. 2017;20:8–24
Ferrari S, Lewiecki EM, Butler PW, et al. Favorable skeletal benefit/risk of long-term denosumab therapy: a virtual-twin analysis of fractures prevented relative to skeletal safety events observed. Bone. 2020;134:115287.
copyright © 2025 CCRN
Any views expressed above are the author's own and do not necessarily reflect the views of CCRN.